Sometimes, It’s Okay not to be Okay
There are no silver linings with this pandemic. There are, however, insights, opportunities, and new perspectives being realized as this virus continues to ravage our country and healthcare resources. COVID-19 has undeniably and understandably strained healthcare workers – the armor of invincibility is wearing thin. Many are speaking out about this from a first person narrative, sharing their own stories of distress, anxiety, depression. Being a healthcare worker in the time of COVID-19 has normalized burnout, given permission for clinicians to dress themselves in the language of mental health more freely, incur less stigma and all but removed concern for negative consequences. This is good news indeed, as it is hard to change something until it is recognized as a problem.
But this is not a new problem. Depression, anxiety, substance misuse, marital discord, adjustment reactions … all of these are common among health professionals before COVID-19. True, this pandemic is worsening the incidence of mental health issues and it is allowing a conversation that is typically relegated to hallway whispers or private journal entries to finally happen in public.
A few years ago, my daughter asked why I am seeing patients in a new location. When I explained that I see doctors as patients now, she said, “Oh, that makes a lot of sense because they were just like regular people before they became doctors.” Right. Becoming a doctor is not an antidote to being human. Yet sometimes we expect superhuman qualities from physicians and one of those is to be immune from mental health disorders. In fact, there are good reasons many physicians hide this type of suffering and are reluctant to seek care. In a recent survey, as many as 40% doctors report reluctance to seek formal care for a mental health condition as the result of licensing concerns which presents a substantial barrier to treatment and is sadly still a realistic fear. A recent review of medical licensing applications found that just 53% of states ask questions limited to functional impairment and only 14% of applications limited their inquiries to current problems. Of note, these questions are out of compliance with the Americans with Disabilities Act and this finally led the Federation of State Medical Boards and the AMA House of Delegates (in June, 2018) to recommended that ALL state medical licensing applications adopt the following language, “Are you currently suffering from any condition for which you are not being appropriately treated that impairs your judgment or that would otherwise adversely affect your ability to practice medicine in a competent, ethical and professional manner? (Yes/No).” This could be a game changer for reducing one barrier to seeking care for mental health concerns among physicians and physicians in training.
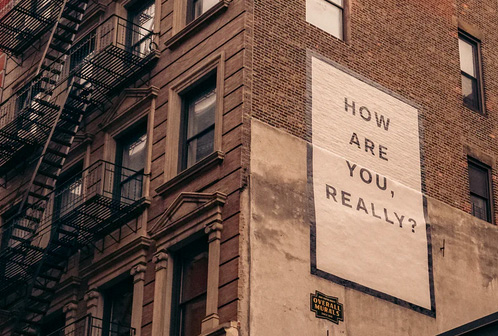
The other barriers will only slowly disintegrate through honest conversations, acknowledgement that all health professionals are first human beings and thus subject to the full continuum of human experience, and a celebration of help seeking as a sign of strength and courage, not weakness. Sometimes, it really is okay not to be okay. What is not okay is to hide it, refuse to talk about it, or to get help. So, I am asking, “How are you, really?”
About Tend Health
At Tend Health, our mission is to ensure all healthcare professionals have access to exceptional mental health care. We partner with organizations and training programs to provide low-friction, human-centered, and highly specialized support. Our doctoral-level clinicians also provide private one-on-one counseling and coaching for health professionals. Get in touch today to learn more.
 We love staying connected to our community.
We love staying connected to our community.
 Tina Runyan, PhD, ABPP
Tina Runyan, PhD, ABPP